Good nutrition during pregnancy is more about the quality of food eaten than the quantity. Pregnant women need a healthy and balanced diet that incorporates five food groups:
a) Wholegrains including wholemeal bread, brown rice, pasta, oats, barley, quinoa.
b) Choose lean protein from meat, poultry, fish, eggs, beans, soy products, nuts and
c) Eat a variety of protein every day
d) Dairy products including milk, yoghurt and cheese. Choose low fat or fat-free dairy
e) All types of fruits
f) A variety of colourful vegetables
Half your plate with fruits and vegetables during mealtimes. Oils and fats are another part of healthy eating. During pregnancy, the fats that pregnant mother eat provide energy and build the placenta. Healthy fats including avocados, nuts and seeds as well as vegetable oils such as sunflower oil, canola oil, olive oil, etc. are essential.
Calories
During the first trimester with one baby, usually, no extra calories are needed. In the second trimester, pregnant women need an additional 280 calories per day. In the third trimester, about 470 extra calories a day.
Key nutrients for a healthy pregnancy
- Folate or folic acid: Folic acid prevents neural tube defects. Pregnant women should
- consume at least 600 mcg of folic acid each day. Food sources of folate include legumes, green leafy vegetables, citrus fruits, folate fortified cereals, pasta and bread.
- Iron: Maternal iron deficiency is the most common nutritional deficiency during
- Pregnant women need at least 29 mg of iron each day. Foods rich in iron
- include red meat, chicken, fish, legumes, spinach, iron-fortified bread and cereals.
- Calcium: During pregnancy, calcium is needed for the healthy development of a baby’s teeth, bones, heart, nerves and muscles. During pregnancy, the recommended amount of calcium is 1,300 mg per day for 13 to 19 years old and 1,000 mg per day for women aged 20 to 50. That means at least three daily servings of milk, yoghurt or cheese.
- Vitamin or mineral supplementation may be needed to ensure pregnant women get
- enough folic acid, iron and other nutrients.
Safe foods for Pregnancy and What to Avoid
Most foods are generally safe. However, pregnant women and their unborn children are more susceptible to food poisoning. To reduce the risk of foodborne illnesses, pregnant women are advised to avoid the foods below:
- unpasteurized milk, including goat’s milk and foods made of unpasteurized
- milks
- soft cheeses; hard cheeses are safer to consume
- unpasteurized fruit or vegetable juices. Unpasteurized juice must be boiled for
- at least 1 minute
- raw or undercooked meat, poultry, eggs, fish or seafood
- raw sprouts
- alcohol consumption
- also, avoid tasting raw dough or batter
Vegetarian Diets
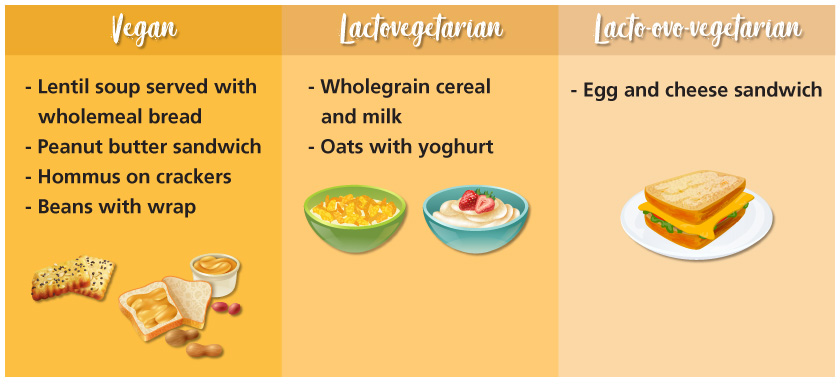
A vegan (strict vegetarian) eliminates all dietary sources of animal protein such as meat, poultry, fish, eggs and dairy products. An ovo-vegetarian consumes eggs (exclude meat, poultry and fish) while a lactovegetarian consumes milk, cheese and other dairy products (exclude meat, poultry, fish & eggs). On the other hand, a lacto-ovo-vegetarian consumes eggs and dairy products (exclude meat, poultry and fish).
The more restrictive the diet, the more challenging it is to ensure adequacy. The vegan diet is a little more complicated but can be adequate with some planning. Ensure a well-planned vegetarian diet, so that it can meet the nutritional needs of a pregnant woman. Vegetarians should also pay special attention to ensure that they get adequate protein, calcium, iron, zinc, vitamin B12 and vitamin D.
Protein:
Proteins from animal sources such as meat, poultry, fish, eggs, and dairy products contain essential amino acids that are complete proteins. There are also plant-based proteins such as lentils, legumes and cereals, but these are incomplete proteins. Combining two or more of these incomplete proteins together forms a complete protein, also known as complementary proteins.
The most common combination of complementary proteins is
i. Grains with lentils / legumes / nuts / seeds
ii. Grains with dairy products / eggs
Example:
Calcium helps foetal bone growth.
Calcium-rich foods include broccoli, legumes, tofu, almonds, sunflower seeds, chia seeds, calcium-fortified cereals and juices.
Iron prevents anaemia.
High iron foods include legumes, leafy vegetables (i.e., spinach), iron-fortified bread and cereals. For pregnant women who are vegetarians, they can increase iron absorption by combining plant-based iron sources with vitamin C rich foods.
Zinc:
Usually found in animal foods. Vegetarians can include wheat germ, tofu, nuts (cashews, and almonds), seeds (sunflower, chia seeds), beans and fortified breakfast cereals to increase zinc intake.
Vitamin B12:
Usually found in animal foods, vitamin B12 is not a nutrient of great concern for vegetarians who regularly consume eggs or dairy products (lacto-ovo-vegetarians / lacto vegetarians / ovo vegetarians). Vegans should include vitamin B12 fortified soymilk and breakfast cereals.
Vitamin D:
Foods containing vitamin D include fortified soy milk or nut milk. The other primary source results from sunlight exposure, causing vitamin D to be synthesized in the skin.
Fish
Large and deep-sea fish can contain high levels of mercury, which has been linked to birth defects. To reduce the risk of birth defects, pregnant women should limit their intake of fish high in mercury:
- Shark (flake)
- Marlin
- Swordfish
- Orange roughy (sea perch)
- Bigeye tuna
- King mackerel
- Tilefish
Consensus guidelines have recommended that pregnant women consume at least 200 mg of DHA per day, which they can achieve by consuming 2 to 3 servings of low mercury seafood per week. These include:
- Herring
- Salmon
- Sardine
- Trout, freshwater
- Tilapia
- Whitefish
- Butterfish
- Black sea bass
- Clam
- Crab
- Oyster
- Scallop
- Shrimp
- Squid

Caffeine is a stimulant found in tea, coffee, soft drinks, chocolate, energy drinks and some over-the-counter medications. Coffee is one of the most common sources of high caffeine intake. During pregnancy, caffeine clearance from the mother’s blood slows down significantly. Lowering daily caffeine intake during pregnancy is recommended by WHO for pregnant women who frequently consume high daily caffeine intake (more than 300 mg per day). This reduces the risk of pregnancy loss and low birth weight neonates.
Caffeine intake of less than 200 mg daily appears to be safe for pregnant women to consume. That is roughly the amount of caffeine in 2 cups of brewed coffee, five cans of cola or one energy drink. Please keep in mind that actual caffeine content in beverages varies widely, especially among energy drinks.
* Macronutrients (calories, protein) and micronutrients (folic acid, iron, calcium) requirements based on Recommended Nutrient Intakes for Malaysia 2017
Dietitian
Sri Kota Specialist Medical Centre (SKSMC)